Attorneys for Tulare Regional Medical Center (TRMC) are back in court as the trial between the hospital and its former medical executive committee (MEC) continues in its second week – after nearly a month’s break.
Lawyers for the former MEC and medical staff claim that the move to replace them was unlawful and retaliatory, while lawyers for the hospital contend it was not only appropriate but necessary to keep the hospital’s doors open.
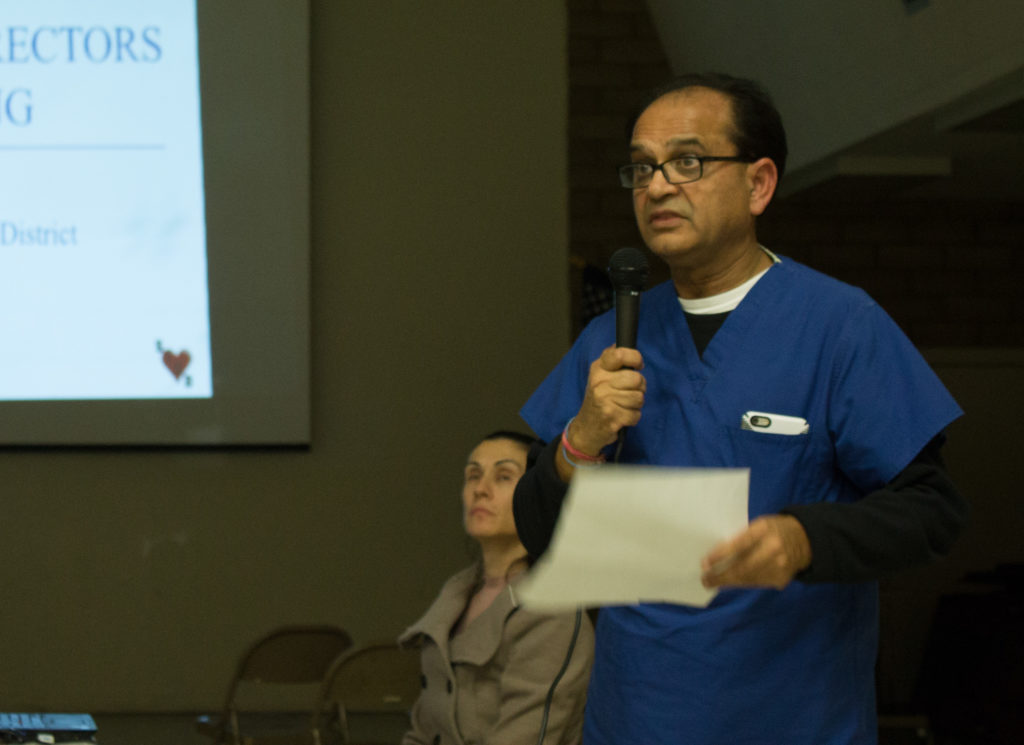
Dr. Parmod Kumar took the stand Wednesday, testifying for the hospital’s defense in the suit. Kumar, a long-time hospital board member currently facing a recall election, has emerged in testimony throughout the suit as a pivotal figure in creating the new medical staff.
Meeting At A Friend’s
After providing testimony on cross-examination, the judge in the case, Hon. David Mathias, asked Kumar about a point that had came up — drafting bylaws and rules for the new medical staff.
Kumar told Mathias that the bylaws were created before the Jan. 26 board meeting in which board members, with Kumar abstaining, voted to install a new medical staff/executive committee.
The core group of the medical executive committee, Kumar told the court, had met to decide a path forward after what hospital administrators considered a disastrous verbal report from Dr. Everett Davis, an inspector with the California Department of Public Health.
Davis was acting as an inspector for the Center for Medicaid and Medicare Services, and met with Kumar and hospital administrators during the first week of January 2016 to deliver the results of a CMS inspection.
Terri Keville, a healthcare attorney with specializations in medical staff and peer review work, testified as an expert witness for the hospital Wednesday. She stated that she felt the hospital board’s actions were justified, given the perceived urgency.
A February 2, 2016 letter to the hospital stated that CMS required not only a course of action but clear evidence that the hospital had corrected the various issues found by Davis survey — inclusive of, but not limited to, medical staff issues — by February 13, 2016, or it would face the loss of its Medicare accreditation by May 2016.
“While it’s true that it’s unusual for a hospital to be decertified by Medicare, it’s not unheard of,” Keville told the court. “It was my impression that the board felt here with the existing medical staff leaders that there was absolutely no way they could timely remedy the problems that were outlined [in the report], and that had been expressed, summarized by the surveyor in the exit conference.”
Another expert witness, Dr. Allan Pont, testified for the hospital during Thursday’s afternoon session, John Harwell, an attorney for the former MEC, asked Pont, to summarize his opinion of the hospital’s reaction at the conclusion of the CMS survey exit interview. Pont served in various hospital administrative positions, most recently as Chief Medical Officer at California Pacific Medical Center in San Francisco.
Pont said that it was his opinion that “the CEO [Dr. Benny Benzeevi] and MSO [Evelyn Vallarta] had a panic attack,” likely due to the gravity of Davis’ findings combined with a lack of experience. He stated that the letter’s strict tone and requests, believed to be an imminent and immediate threat, were standard, boilerplate language.
“Very few hospitals close so quickly,” Pont said.
Before the board even had the letter in its hands, Kumar said he felt he had to act to save the hospital from closure.
Kumar and the rest of the group met at former Tulare City Councilmember Skip Barwick’s home, he told the court, and it was there that Kumar decided to move forward with the creation of the medical staff’s structure and bylaws.
View note“The decision was made at that meeting at Mr. Barwick’s house, we’re going to go forward with the medical staff,” Kumar said.
Dr. Anthony Trujillo had previously described the meeting as having happened at a home belonging to a friend of Kumar’s, but did not name whose home it was.
Bylaws by BakerHostetler
Kumar said that he reached out to Bob Wolin, a Houston-based attorney and partner at the BakerHostetler law firm, to draw up the new medical staff’s bylaws and regulations.
BakerHostetler is a national firm, headquartered in Cleveland with 13 other offices, that both the Tulare Local Healthcare District (TLHCD) the entity which owns TRMC, and Healthcare Conglomerate Associates (HCCA) the firm which runs TRMC, use for various legal services.
Wolin currently works with the hospital, and has worked with the hospital in responding to surveys from the Center for Medicare and Medicaid Services (CMS) and the California Department of Public Health. A separate BakerHostetler attorney, Bruce Greene, attends the hospital’s board meetings and previously handled Public Records Act requests.
The idea to utilize Wolin came after seeing his work with the hospital in dealing with the CMS survey that would later serve as the catalyst for the removal of the former medical staff, Kumar told the judge.
“I had one discussion with him and then it is always prepared by a lawyer in the past,” Kumar said. “So I made that call to him.”
Kumar said he made the call in his capacity as a member of the medical staff.
“Can any member of the medical staff call BakerHostetler,” Mathias asked, “and incur expense, such as drafting bylaws?”
Kumar stated that the medical staff was allowed to call their lawyers at any time they wished — but Mathias noted that, at the time he had called on Wolin, the new medical staff did not yet exist.
“So prior to the new medical staff being approved, prior to the board of directors even knowing that this was going to come before them, you had initiated BakerHostetler to draft 280 pages of documents in preparation for something you didn’t even know was going to happen at the time,” Mathias said.
Kumar replied that he did so as a process of “getting ready” if the ouster of the former staff were to happen, since Davis took issue with the lack of updates to the medical staff bylaws.
View noteAmir later asked who Kumar thought would have paid for the legal fees.
“The payment is customarily made either by the medical staff funds for the lawyers’ bills,” Kumar said, “or the administration.”
“Very Unusual”
Both sides agree that the former MEC’s Chief of Staff did not appear at some — or all — TLHCD board meetings between January 2013 and December 2014.
During the times when the Chief of Staff did not appear, a printed report was provided in lieu of providing anyone to speak to the board in person.
Kumar said that he felt “very uncomfortable” in approving those reports, stating that he would have preferred to dialogue with a representative of the MEC to gain a greater understanding of the issues brought forth by the medical staff.
He stated that there were two efforts made by the board to meet with the medical staff to resolve any issues between them.
One, which Kumar believes happened in the first half of 2015, was a meeting between Dr. Abraham Betre and Dr. Robert Orth of the former MEC, Kumar and Sherrie Bell of the Board of Directors, and Dr. Benny Benzeevi.
Sherie Bell is no longer a board member, and at the time Benzeevi was only the chairman of HCCA; Benzeevi is now the CEO and Chairman of HCCA.
Orth and Betre walked out, Kumar said, because Benzeevi was in the room.
“They didn’t want Dr. Benzeevi,” Kumar said, before he was admonished for stepping beyond the scope of the question asked.
Orth testified to the same in his April 5 testimony — but he stated that the reason he and Betre left was that Benzeevi was not the CEO at the time. He said they hadn’t agreed to Benzeevi’s being at the meeting — only Paul Walker, the acting CEO during that time period.
“We tried to discuss issues, since Mr. Paul Walker set up the meeting, because he was the acting CEO, and Sherrie Bell stated that it was her birthday. So she really wanted to talk to us because she was missing her birthday dinner for this,” Orth said. “We said, ‘We really want to talk to you.’”
“There was discussions on who was the actual CEO at the time, and it was Paul Walker, as far as we knew and as far as the board members knew. [Benzeevi] said he was the new CEO, which was news to us, and we left,” Orth said.
The relationship with the prior MEC was “not good,” but there is now “excellent collegiality” between the MEC and the board, Kumar told the court.
Pending Disciplinary Action
Lawyers for the former Medical Executive Committee have claimed throughout the case that part of the reason the new MEC was formed was that Kumar was facing potential disciplinary action from the former MEC on January 27.
Members of the MEC state that he would have faced suspension of his privileges on that date, but the hospital’s attorneys dispute that.
During Kumar’s direct testimony, he stated that he had never previously been subject to disciplinary action during his work as a military doctor or at prior hospitals.
Kumar was facing discipline from the former MEC over two allegations: inaccurate record keeping and using foul language in front of his colleagues; members of the former MEC had recommended he take recordkeeping courses and anger management counseling.
In early 2014, Rachel Sandhu in the hospital’s medical records office sent Kumar an email to his personal email account.
“I have found two more charts with H&Ps over 30 days, total of five charts for the month of January,” Sandhu wrote to Kumar. “We cannot legally code a chart with H&P over 30 days over. TRMC will not receive any monies for these services.”
View noteThe term “H&P” refers to “history and physical,” defined as “the initial clinical evaluation and examination of [a] patient” by MedicineNet.com; Sandhu’s email would likely refer to the forms generated by such an examination.
Later in the year, Sandhu sent Kumar another email about the same types of forms.
“I have three charts on my desk that were missing H&P chart analysis. Charts now contained short H&Ps with fraudulent dates. The issue will be forwarded to utilization review committee,” she wrote.
Kumar told Amir that he did not recall seeing either email, but that he thought the accusations were unfair and disagreed with them.
“The issue here is that whenever there is a patient who comes for a procedure to the hospital and I have to dictate a note from my office, which is the history and physical, but with the new regulatory insurance coverages, you have to apply for an authorization for the procedure to the insurance company,” Kumar said. “So sometimes that takes more than 30 days because a lot of issues, the insurance companies don’t buy into.”
Kumar said that the prior MEC should have given him the benefit of the doubt.
“So I have to have an authorization for the procedure to be done on a particular time. I can’t otherwise schedule a patient until the procedure has been authorized by the insurance carrier. That takes more than 30 days sometimes. So when I show up to do the case, I have the old history and physical, which I’m not aware of, and 30 days have gone by,” Kumar continued. “So this is really not some sort of a pattern that I have. I’m just a victim of the circumstances.”
In a declaration made in a separate case that Kumar pursued against Dr. Abraham Betre, Kumar had stated that “the ‘backdating’ accusation was made after I had inadvertently listed the dates of my dictation as the dates of three patients’ physical examinations, at a time when I had performed approximately 150 procedures per 18 month.”
Kumar said that he disagreed with the recommendations but eventually took the classes in April; he said he had previously planned to take them before the January 27 deadline, but that the organizers of the recordkeeping classes at UC San Diego had a computer mishap that meant he would not be able to attend.
Kumar also agreed that the prior MEC had also accused him of requiring anger management classes. A letter from the group stated that “it [had] been reported that, one, you used loud and foul language in the nurses’ station that was heard by at least six employees.”
He said those charges were unfair, too.
“That’s not me,” Kumar said. “The MEC never showed me anything on their behalf to build a case against me. I never saw any document. I never [knew] the names.”
During direct examination, Kumar stated that he saw a psychiatrist in November 2015 to satisfy the requirements of the old MEC.
View noteHowever, Kumar’s declaration in the Betre case appears to refer to Kumar seeking anger management classes after the new MEC was formed; it was not made clear in that declaration clear whether he sought additional, separate classes, or simply turned over existing proof of completion to the new group.
“I insisted that I take the anger management class, the recordkeeping class, and see a psychiatrist, so to avoid any I claim of bias or impropriety by Dr. Betre or the former MEC in the future. The new MEC agreed, and I presented proof of compliance to the new MEC, which then formally closed the ‘investigation,’” Kumar wrote.
Separately, Dr. Ronald Ostrom, Chief of Staff of the new MEC, stated the same.
“…Dr. Kumar voluntarily took an anger management class and saw a psychiatrist anyway. After Dr. Kumar presented documentation that he had done so, the current MEC formally closed the peer review matter against him,” Ostrom wrote.
Joseph Oldenbourg contributed to this report.